Every child carries unique potential that’s actualized with the right nurture and support. For children with special needs, well-chosen interventions can be especially powerful in supporting their development.
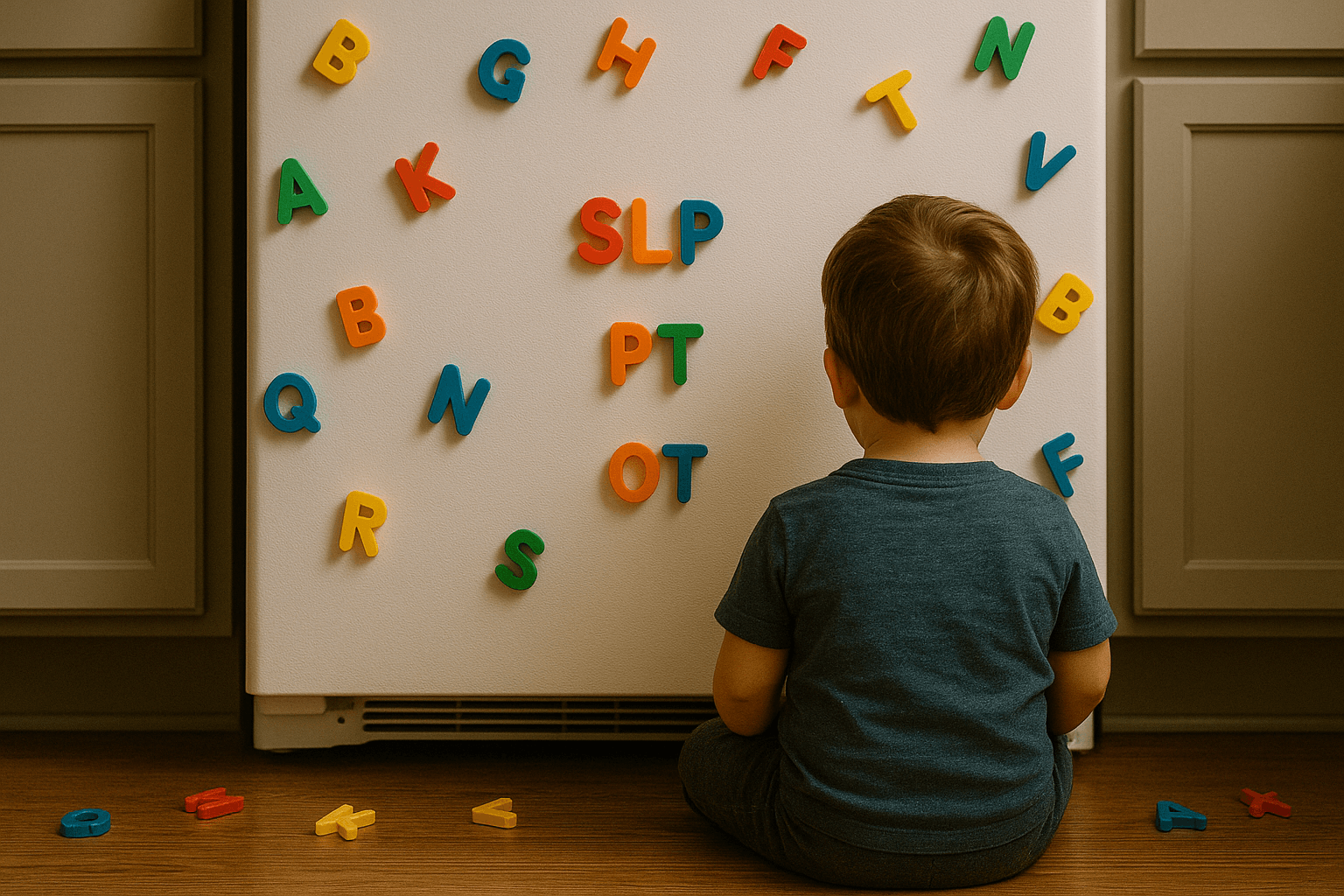
The variety of available therapy options (and their abbreviations) can be overwhelming. This guide offers a clear snapshot of common therapies, so you can feel confident and empowered as you explore what’s best for your child.
Remember, children thrive best when intervention decisions are made in partnership with trusted professionals.

Caring for a child with special needs affects everyone.
Our Siblings Are Special Too guide shares ten grounded, actionable ways to support siblings with sensitivity.
EI - Early Intervention
Early intervention is a program for infants and toddlers (birth to 3 years) who have developmental delays or disabilities. It provides a combination of therapies and supports to help children develop critical skills.
When to pursue: Consider EI for concerns around developmental delays in any area – physical, cognitive, communication, social-emotional, or adaptive – detected before age 3. The earlier the intervention, the better the developmental outcomes.
What does it look like? A team of providers (PT, OT, SLP, etc.) coaching the parents and working with the child directly, often by coming into the home or daycare.
ABA - Applied Behavior Analysis
ABA is a widely used therapy, especially for children with autism. It involves breaking down skills into small, manageable steps and teaching them using repetition and reinforcement techniques. The structured approach helps improve social skills, communication, and behavior.
When to pursue? It’s recommended to begin ABA soon after diagnosis or when behavioral and social delays are observed, often starting in early childhood, to maximize outcomes.
What does it look like? ABA uses repetition, prompts, and positive reinforcement, through structured activities or games, puzzles, and role-play.
PT - Physical Therapy
Physical therapy focuses on improving a child's gross motor skills, such as crawling, walking, balance, and coordination to increase mobility and independence in daily activities.
When to pursue: If a child shows delays in motor milestones (sitting, crawling, walking) or has muscle weakness, low tone, or motor coordination difficulties. Therapy can begin in infancy, or whenever challenges emerge.
What does it look like? The therapist uses guided exercises using tools like balance boards, therapy balls, obstacle courses, and resistance bands.
OT - Occupational Therapy
Occupational therapy helps children develop fine motor skills and improve their ability to perform everyday tasks, such as dressing, eating, or writing. OT can also address sensory processing issues to help children better handle everyday sensations.
When to pursue: If delays or difficulties appear in fine motor tasks, sensory sensitivities, or daily living skills. It’s often started when a child is very young, though it can be helpful at any stage when support is needed.
What does it look like? Therapists use small toys like blocks, beads, playdough, crafts, sensory bins, and adaptive tools like non-slip mats, larger utensils and textured grips.
SLP - Speech Language Pathology
Speech therapy assesses and treats speech, language, and communication difficulties. It helps with articulation, fluency, voice, and social communication.
Specialized SLPs can also provide feeding therapy for children who have difficulties with eating and swallowing. They may practice safe swallowing and gradually introduce and build comfort with different textures.
When to pursue: If a child demonstrates delays or difficulties in speech development, language comprehension, feeding, or swallowing, reach out to an SLP. It’s ideal to pursue as young as possible, from early intervention through early childhood.
What does it look like? Practicing sounds, words, and social communication through songs, picture cards, stories, and play; it may also include feeding therapy with textured foods, straws, and safe-swallow strategies.
CCPT - Child-Centered Play Therapy
CCPT is a non-directive therapy where children use play as a natural medium to express feelings and solve problems. The therapist creates a supportive environment and follows the child’s lead, using the play to generate a process of growth and healing.
When to pursue: Play therapy can be beneficial when a child shows emotional or behavioral challenges, difficulty expressing feelings, or after trauma.
What does it look like? Play therapy takes place in a supportive playroom where the child leads with toys, art, and role-play while the therapist reflects, validates, and helps them process emotions.
SI - Sensory Integration
Sensory integration therapy helps children who struggle to process and respond to sensory information – sights, sounds, touch, movement, and more. It’s often provided by a specially trained occupational therapist.
When to pursue: If a child is overly sensitive or overwhelmed by sounds, textures, or movement; craves constant motion or deep pressure; or has difficulty focusing and regulating emotions because of sensory processing challenges they’ll likely benefit from SI.
What does it look like? The therapist uses play-based activities designed to help the child regulate and organize sensory input, such as swinging, jumping, climbing, using weighted blankets or vests, tactile play with sand, water, or textured bins, and activities that provide deep pressure or joint compression.
There are many more specialized therapies and supports available as your child's needs evolve. Trust your instincts as a parent, ask questions, and build relationships with professionals who truly listen to your concerns.
Your child's path may look different from others, but with the right support team and advocacy, they can reach their fullest potential.
To get support on your child's developmental journey, reach out to our services specialists. Our team will help you understand your eligibility and connect you with the services that are right for you.

 OPWDD Guidance
OPWDD Guidance Family Support
Family Support Services for Children
Services for Children Services for Adults
Services for Adults Services for Children 0-3
Services for Children 0-3 Adult Acute Care
Adult Acute Care











.png)



.png)